What is person-centred care and how is QMU’s research in this field informing Person-Centred Practice across the globe?
At QMU we are proud of our aim to be world-leading centre for research and development in person-centred practice with a focus on innovative new knowledge in nursing and healthcare.
For many outside the field, however, the term can seem confusing – isn't ALL nursing and healthcare practice “person-centred”?
Surprisingly, no. Person-centered care and the concept of person-centered practice is a relatively new model of practice developed in the second half of the 20th century and QMU’s Person-Centered Practice Framework is the result of empirical research published between 2000-2010.
So what is Person-Centred Care?
At its core, Person-Centred Care is an approach to healthcare, support and treatment that focuses on the individual.
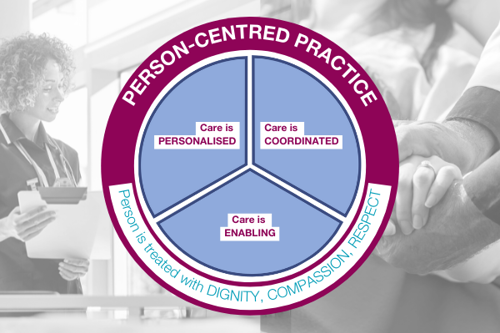
It rests on four key principles:
- Care is personalised – putting the individual’s needs and preferences (patient, practitioner, local community member) at the heart of the care plan.
- Care is coordinated – all medical staff and care staff treating an individual work together to deliver a smooth and effective care plan.
- Care is enabling – the individual receiving treatment and care has the power and support to make their own informed decisions.
- The individual is treated with dignity, compassion, and respect.
What research has QMU developed to address and influence Person-Centred Care?
The PCPF developed by QMU researchers is currently the most adopted framework for informing the development of person-centred practices and systems in different healthcare settings globally.
Through influential participatory research and development with multiple partners across the UK, Europe, USA, Canada and Australia, six evaluation instruments and one observational tool were developed, which helped identify key outcomes from the implementation of Person-Centred Practice.
Examples include:
- In nursing home settings, research and development projects have results in improvements to the care environment, greater resident satisfaction, improved staff wellbeing, reduction in falls and the reduced use of psychotropic medications.
- In palliative care, evaluations of practice development programmes have shown improvements in regulatory quality indicators, improvements in the quality-of-care environments, better staff communication, increased staff development and retention.
Key performance indicators (KPIs) relating to person-centered practice in nursing, developed through various strands of our research, have been tested in a number of clinical settings.
Positive findings from these tests confirm that a patient’s care experience is enhanced when nurses are engaged in delivering person-centered care.
How is this research making a difference today?
Our research is being applied in many areas of care, but below is one example we are proud of.
In the Republic of Ireland, a national programme of development was commissioned by the Health Service Executive (HSE) across the Irish health system (2017-2020) focusing on the creation of person-centered cultures.
Two-hundred facilitators were embedded in the health system to facilitate practice change.
Positive impacts include a move towards more person-centered practices (e.g., changes to language used in practice, better staff relationships); more effective communication in and between teams; and innovations in practice such as new services and improved quality assessments from regulation authorities.
As a result of this work a ‘practical’ set of person-centered principles were developed and these, along with the PCPF have been integrated into the Health Service Executive’s ‘Health Services Change Guide.’
Read the full person-centred care case study here.
In this video, Professor Brendon McCormack talks about using a theory of person-centredness to transform nursing and healthcare cultures







